Pulp removing for teeth number 6 and 7
The pulp of the tooth is a part that contains nerves and many blood vessels located beneath the enamel layer of the tooth. When the pulp is damaged, it affects the oral health and weakens the tooth. Root canal treatment is a procedure to replace lost, damaged, or infected parts of the tooth, helping to alleviate pain and improve dental care. So how is the pulp removing for teeth number 6 and 7 performed?
Learn about the pulp removing for teeth number 6 and 7
Basically, pulp removing for teeth number 6 and 7 is performed like other teeth.

The dental pulp is the inner part of the tooth responsible for supplying nutrients to the tooth. Inside it are nerve fibers and blood vessels, which are protected by the tooth enamel and dentin. The dental pulp consists of two parts: the pulp chamber and the root canals. When the dental pulp is damaged, it negatively affects the structure of the tooth, leading to a lack of sufficient nutrition in the long term. At this point, your tooth will weaken, requiring examination and surgery to remove the inflamed pulp.
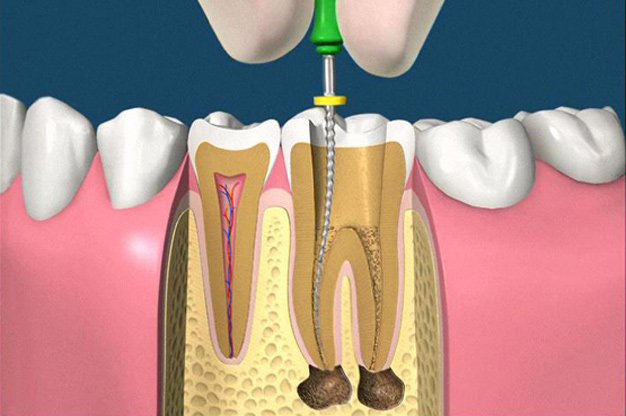
Root canal treatment is the process of removing damaged, inflamed, or infected pulp from inside the tooth, followed by thoroughly cleaning the root canals and sealing any openings with specialized filling materials such as gutta-percha, composite resin, or ceramics. When the pulp of the tooth is inflamed and not promptly treated, it can lead to prolonged episodes of pain and eventual loss of the tooth.
When undergoing the procedure of root canal treatment, you will be administered local anesthesia in the area of the affected tooth, so you don’t need to worry about experiencing pain. After completion, you will no longer feel much pain or discomfort in the tooth because it gradually loses connection with the central nervous system. If you experience any pain after the pulp removal, it’s important to promptly consult a dentist for diagnosis and timely treatment of any complications that may arise.
How much does gum contouring cost? When is it recommended to undergo gum contouring?
What is a pulp inflammation? Is it serious?

- Unusual discoloration of the tooth (mainly in deep teeth causing it).
- Toothache in episodes, especially more at night, with large black holes on the tooth.
Should you have pulp removing for teeth number 6 and 7?
Which cases require pulp removing for teeth number 6 and 7?
- Persistent pain in the tooth area, accompanied by bleeding upon touch.
- Severe tooth decay leading to pulpitis.
- Pain spreading from the mouth to the ears, especially at night, with ineffective medication.
- Increased sensitivity of wisdom teeth to spicy, cold, and sour foods, often causing pain and discomfort.
- Swelling and redness in the cheek area, indicating inflammation.
- Formation of white abscesses under the tooth roots, causing severe pain upon touch and potential unpleasant mouth odor.
Does pulp removing for teeth number 6 and 7 hurt?
Pulp removal may involve some discomfort, but with the use of local anesthesia, the procedure is typically not painful. The area around the tooth is numbed before the procedure, ensuring that you don’t feel pain during the pulp removal process. After the procedure, you may experience some soreness or discomfort, but this can usually be managed with over-the-counter pain medication as directed by your dentist. Overall, while the idea of pulp removal might sound intimidating, the actual procedure is generally well-tolerated with minimal discomfort.
Pulp removing for teeth number 6 and 7
Normally, getting the pulp of the molars will take longer than the incisors because the position of the teeth is quite difficult to perform the treatment and the anatomy of the molars also contains more canals.
It is very necessary to conduct a damaged tooth pulp, otherwise the infection will spread and cause dull pain for the patient. Carrying out marrow extraction needs to be done at specialized medical facilities and must ensure the correct procedure, otherwise, the inflamed pulp will not be removed, causing the patient to suffer pain and proceed to take the marrow again. It is also expensive for the patient, affecting the health of the teeth.
Technical standards for taking root canals are as follows:
Examination:
After listening to the patient tell about his symptoms, the dentist will allow the patient to conduct a number of methods to serve the root canal such as:
- X-ray – dental x-ray: helps to determine the dark spot on the apex of the tooth that has problems, how the infection has affected the pulp
Determine the fistula to drain pus to see if the pus has escaped or not. Gum boils are usually tender to the touch, but these do not necessarily require pulp. - Identify problem teeth that are darkened: Discoloration of teeth means that some change has occurred in the neural space. In many cases, this sign indicates the need for root canal treatment.
- Nerve contact: Because it is difficult to determine how the nerve is located with the tooth surface, contact of this nerve can occur if the dentist comes into contact with pulp tissue during the procedure. treatment course. In this case, a root canal should be obtained, as exposure can cause tissue degeneration in the future.
Conduct:
- Anesthesia: After conducting the examination, the dentist will give a local anesthetic at the damaged tooth to create a feeling of comfort and good psychology for the patient during the procedure. Moreover, when the treatment is finished, the anesthetic will also wear off, and the patient will not be too affected to his daily activities.
- Put the rubber base: The dental base is a rubber sheet to ensure a dry area around the problem teeth no.6 and no.7. This sole prevents saliva from reaching the treated area.
- Make an opening and remove the infected pulp: The endodontist creates an opening in the crown. After removing the infected tooth pulp 6, 7 to the outside, the doctor continued to reshape the canal. Next is to fill the empty pulp chamber with specialized materials in dentistry. To ensure the teeth from the attack of bacteria and to ensure the aesthetics and shape the space for filling.
- Apply medicine and fillings: After the space is cleaned and shaped, in case your tooth has an internal infection, the dentist will apply medicine to the inner tooth area to remove bacteria, then The doctor will fill the canal with a biocompatible material, usually a rubber-like material called gutta-percha. Gutta-percha is placed with a cementitious layer to ensure complete sealing of the canals. In most cases, a temporary filling is placed to close the gap. The temporary filling will be removed by the dentist before the tooth is restored.
- Restoration: In the final stage, your dentist will completely restore your treated tooth. In many cases, because teeth are more prone to fracture after root canal treatment, your dentist may recommend a root canal and crown. It covers the entire tooth to protect the tooth from further damage. To fit a crown, your dentist must first scrape off some of the enamel on the outside of your tooth. They use strong dental glue to keep it in place. Once fixed in place, it will feel and act like a natural tooth. Of course, the cost of root canals and crowns is higher than root treatment alone, but your dentist will tell you what is best for the condition of your teeth.
Note when treating the pulp of teeth number 6 and 7

After completing the 6 and 7 root canals, the dentist will ask you to perform strict aftercare, usually following the following general rules:
- Take pain relievers when it is too painful. Limit eating until the numbness in your mouth is gone
- Do not chew on the treated tooth until it is completely gone Brush your teeth with fluoride toothpaste and floss daily as usual
You may experience mild pain and soreness after the procedure and during the pulp recovery period, which can last a week or two. Contact your dentist if you experience the following signs:
- Sharp pain after root canal: If you have taken painkillers but still have sharp or severe pain after root canal, chances are Your root canal has not been successful and you should call your dentist right away.
- Swelling after a root canal: Usually swelling and pain are normal after a root canal and will go away after a few days. If symptoms don’t go away, or the pain gets worse, call your dentist.
- Toothache when biting after a root canal: Some discomfort, pain or sensitivity is normal after having your pulp removed. However, if you continue to experience pain when you bite down, it may be because your filling is not flattened enough. You should call your dentist to double check.
- Long-term tooth pain after root canal: Chances are that your tooth may not be able to heal properly after a root canal, or the tooth may have broken or new decay.
- Jaw pain after root canal: Pain in the jaw is normal, if it doesn’t go away or gets worse, you need to call your dentist. Allergic reaction to your medication
- Temporary crowns or your fillings fall out Infections after root canal: Severe pain that gets worse a week after the procedure could be a sign of infection, and you should call your dentist.